Multiple sclerosis (MS) is a chronic autoimmune disease of the central nervous system that affects millions of people worldwide. It is characterized by inflammation, demyelination, and neurodegeneration, leading to a wide range of neurological symptoms and disabilities. Despite advances in disease-modifying therapies, many individuals with MS continue to experience disease progression and debilitating symptoms for which there are limited treatment options.
This article explores the role of stem cell treatments in the management of MS, including the mechanisms of action, types of stem cells used, clinical trials and research findings, patient experiences, challenges and future directions, and ethical and regulatory considerations.
By delving into the current state of stem cell therapy for MS, we aim to provide insights into its potential benefits and limitations and its impact on the future of stem cell treatments for MS patients.
Overview of Multiple Sclerosis (MS)

Multiple sclerosis (MS) is a chronic autoimmune disease affecting the central nervous system, characterized by inflammation, demyelination, and neurodegeneration. It often presents with a wide range of neurological symptoms, including fatigue, weakness, numbness, and difficulty with coordination and balance. The exact cause of MS is not fully understood, but it is believed to involve a combination of genetic, environmental, and immunological factors.
The course of MS can be unpredictable, with periods of exacerbation (relapses) followed by periods of remission. Despite challenges, ongoing research and advancements in treatment offer hope for improving outcomes and quality of life for individuals living with MS.
Stem cell treatment for Multiple Sclerosis has demonstrated healing and repair-promoting properties. These can be derived from other types of stem cells. These hESCs (human embryonic stem cells) – stem cells derived from donated embryos. Mesenchymal stem cells are injected via a lumbar puncture with the hope that they will mature into nerve cells.
Definition and Pathophysiology of MS

Multiple sclerosis (MS) is a chronic autoimmune disease of the central nervous system (CNS), characterized by inflammation, demyelination, and neurodegeneration. In MS, the immune system mistakenly attacks the myelin sheath, a protective covering that surrounds nerve fibers in the CNS, leading to damage and disruption of nerve signals.
This immune-mediated damage results in the formation of plaques or lesions in the brain and spinal cord, which can interfere with the transmission of electrical impulses along nerve fibers.
As a result, individuals with MS may experience a wide range of neurological symptoms, including fatigue, weakness, numbness, tingling, balance problems, vision changes, and cognitive impairment.
The exact cause of MS is not fully understood, but it is believed to involve a complex interplay of genetic, environmental, and immunological factors.
While there is currently no cure for MS, disease-modifying therapies can help manage symptoms, reduce relapses, and slow disease progression by modulating the immune response and promoting the repair of damaged tissues.
Symptoms and Progression of the Disease

Multiple sclerosis (MS) manifests with a diverse array of symptoms and can exhibit varying patterns of progression, depending on individual factors and disease subtypes.
Common symptoms include fatigue, weakness, sensory disturbances (such as numbness or tingling), impaired coordination and balance, muscle stiffness or spasms, vision problems (such as blurred vision or double vision), cognitive dysfunction (including memory problems and difficulty concentrating), and bladder and bowel dysfunction.
The progression of MS can be unpredictable and may follow different patterns. These vary from patient to patient and everyone is different. However, some common issues may include:
Relapsing-remitting MS (RRMS)
This is the most common form of MS, characterized by periods of symptom exacerbation (relapses or flares) followed by periods of partial or complete symptom resolution (remissions). Relapses can occur suddenly and may last for days to weeks before symptoms improve. Between relapses, individuals may experience periods of stability with minimal or no symptoms.
Secondary progressive MS (SPMS)
In SPMS, the disease typically transitions from a relapsing-remitting pattern to a progressive course, with a gradual worsening of symptoms and disability over time. Relapses may occur less frequently, and there may be fewer periods of remission. SPMS often develops in individuals with RRMS after several years of disease progression.
Primary progressive MS (PPMS)
PPMS is characterized by a steady progression of symptoms and disability from the onset of the disease, without distinct relapses or remissions. Symptoms may worsen gradually over time, leading to increasing disability and functional impairment.
Progressive-relapsing MS (PRMS)
PRMS is a less common subtype of MS characterized by a progressive worsening of symptoms from the onset of the disease, with occasional relapses or flare-ups that may or may not result in symptom improvement.
MS can also lead to complications such as muscle weakness, spasticity, mobility limitations, pain, depression, and cognitive impairment, which can significantly impact quality of life.
The progression of MS varies widely among individuals, and the course of the disease can be influenced by factors such as age at onset, disease severity, response to treatment, and overall health status. Regular monitoring and management of symptoms are essential for optimizing outcomes and improving the quality of life for individuals living with MS.
Role of Stem Cell Therapy in MS Treatment
Stem cell therapy holds promise for revolutionizing the treatment of multiple sclerosis (MS) by addressing the underlying mechanisms of the disease and promoting tissue repair and regeneration. Here’s an overview of the role of stem cell therapy in MS treatment:
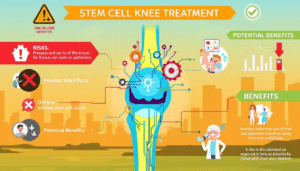
Immunomodulation: Stem cell therapy has immunomodulatory effects, which can help modulate the immune response responsible for attacking myelin and causing inflammation in MS. Mesenchymal stem cells (MSCs), in particular, have been shown to suppress aberrant immune responses and reduce inflammation in preclinical and clinical studies.
Promotion of Tissue Repair: Stem cells can differentiate into various cell types and promote tissue repair and regeneration. In MS, stem cell therapy aims to replenish damaged cells, stimulate remyelination of nerve fibers, and restore normal functioning of the central nervous system.
Neuroprotection: Stem cells secrete neurotrophic factors and other neuroprotective molecules that can support the survival of neurons and protect against neurodegeneration. By providing a supportive microenvironment for neural cells, stem cell therapy may help preserve existing neuronal function and prevent further damage in individuals with MS.
Induction of Immunological Tolerance: Stem cell therapy has the potential to induce immunological tolerance to myelin antigens, thereby preventing further autoimmune attacks on the central nervous system. This tolerance induction may help stabilize the disease course and reduce the frequency and severity of relapses in individuals with MS.
Enhanced Neurological Function: Clinical trials investigating stem cell therapy for MS have reported improvements in neurological function, including reductions in disability scores, improvements in mobility and cognitive function, and decreased disease activity on imaging studies. While results vary among individuals, stem cell therapy offers hope for enhancing quality of life and functional outcomes in MS patients.
Overall, stem cell therapy represents a promising avenue for MS treatment by targeting the underlying disease processes, promoting tissue repair, and modulating the immune response.
Ongoing research and clinical trials are needed to further elucidate the safety, efficacy, and long-term outcomes of stem cell therapies in MS and to optimize treatment protocols for individuals with this challenging disease.
Types of Stem Cells Used in MS Treatment
Several types of stem cells have been investigated for their potential therapeutic use in treating multiple sclerosis (MS). Here are some of the main types:
Mesenchymal Stem Cells (MSCs)
MSCs are multipotent stem cells that can differentiate into various cell types, including bone, cartilage, and fat cells. They have immunomodulatory properties, making them attractive candidates for MS treatment. MSCs can suppress the inflammatory response and promote tissue repair and regeneration in the central nervous system. They also secrete factors that support neuronal survival and reduce neuroinflammation.
Hematopoietic Stem Cells (HSCs)
HSCs are found in bone marrow and can give rise to all blood cell types, including immune cells such as T cells, B cells, and macrophages. Hematopoietic stem cell transplantation (HSCT) involves replacing the immune system with healthy stem cells to reset the immune response and prevent further attacks on the myelin sheath in MS.
Induced Pluripotent Stem Cells (iPSCs)
iPSCs are generated by reprogramming adult cells, such as skin cells, to a pluripotent state, where they can differentiate into any cell type in the body. iPSCs offer the potential to create patient-specific stem cell lines for personalized MS therapies. They can be differentiated into neural progenitor cells or oligodendrocyte precursor cells for transplantation into the central nervous system.
Neural Stem Cells (NSCs)
NSCs are found in various regions of the adult brain and have the capacity to differentiate into neurons, astrocytes, and oligodendrocytes. Transplantation of NSCs aims to replace damaged or lost cells in the central nervous system and promote remyelination of demyelinated axons in MS lesions.
Embryonic Stem Cells (ESCs)
ESCs are pluripotent stem cells derived from the inner cell mass of early-stage embryos. While ESCs have the potential to differentiate into any cell type in the body, ethical considerations and the risk of tumor formation limit their use in clinical applications for MS.
Each type of stem cell has its advantages and limitations in MS treatment, and ongoing research is needed to determine the optimal sources, delivery methods, and treatment protocols for achieving the best outcomes for individuals with MS.
Potential Benefits of Stem Cell Therapy for MS
Stem cell therapy holds significant promise for the treatment of multiple sclerosis (MS), offering potential benefits for individuals living with this challenging disease. Here are some of the potential benefits of stem cell therapy for MS:
Immunomodulation
Stem cells, particularly mesenchymal stem cells (MSCs), have immunomodulatory properties that can help regulate the immune response responsible for attacking myelin and causing inflammation in MS. By modulating the immune system, stem cell therapy may help reduce disease activity, prevent relapses, and slow the progression of MS.
Promotion of Tissue Repair and Regeneration
Stem cells have the ability to differentiate into various cell types and promote tissue repair and regeneration in the central nervous system. Stem cell therapy aims to replenish damaged cells, stimulate remyelination of nerve fibers, and restore normal functioning of neural circuits, potentially improving neurological function and reducing disability in individuals with MS.
Neuroprotection
Stem cells secrete neurotrophic factors and other neuroprotective molecules that can support the survival of neurons and protect against neurodegeneration. By providing a supportive microenvironment for neural cells, stem cell therapy may help preserve existing neuronal function and prevent further damage in individuals with MS.
Disease Modification
Stem cell therapy has the potential to modify the underlying disease processes in MS by targeting immune-mediated inflammation, promoting tissue repair, and restoring homeostasis in the central nervous system. Unlike traditional disease-modifying therapies, which primarily aim to manage symptoms, stem cell therapy offers the potential to address the root causes of MS and alter the course of the disease.
Improved Quality of Life
Clinical trials investigating stem cell therapy for MS have reported improvements in various aspects of quality of life, including reductions in disability scores, improvements in mobility and cognitive function, and enhanced overall well-being. By targeting the underlying disease processes, stem cell therapy may offer hope for enhancing the quality of life and functional outcomes in individuals living with MS.
While the potential benefits of stem cell therapy for MS are promising, further research and clinical trials are needed to fully elucidate its safety, efficacy, and long-term outcomes. Challenges such as patient selection, optimal cell sources, treatment protocols, and standardization of outcomes assessments must be addressed to maximize the therapeutic potential of stem cell therapy for MS.
Frequently Asked Questions

What are stem cell treatments for MS, and how do they work?
Stem cell treatments for MS involve the use of various types of stem cells, such as mesenchymal stem cells (MSCs) or hematopoietic stem cells (HSCs), to modulate the immune response, promote tissue repair, and regenerate damaged cells in the central nervous system.
What types of stem cells are used in MS treatment?
Different types of stem cells, including MSCs, HSCs, neural stem cells (NSCs), and induced pluripotent stem cells (iPSCs), have been investigated for their potential therapeutic use in MS treatment. Each type of stem cell has unique properties and mechanisms of action.
What is the evidence supporting the use of stem cell therapy for MS?
While preliminary studies and clinical trials have shown promising results, the evidence supporting the use of stem cell therapy for MS is still evolving. Further research is needed to determine the safety, efficacy, and long-term outcomes of stem cell treatments for MS.
Who is eligible for stem cell therapy for MS?
Eligibility criteria for stem cell therapy for MS may vary depending on factors such as disease severity, disease subtype, age, overall health status, and previous treatments. Patients are typically evaluated by healthcare providers experienced in MS and stem cell transplantation to determine suitability for treatment.
It’s important to remember that stem cell therapies are a new and evolving field of scientific research and treatment. While many clinical trials suggest hope for MS patients, a consultation is required in order to determine if MS cell therapy injections are right for you and your situation.
What are the potential risks and side effects of stem cell therapy for MS?
Like any medical procedure, stem cell therapy for MS carries potential risks and side effects, including infection, bleeding, graft failure, immune reactions, and the development of tumors or other adverse events. Patients should discuss the risks and benefits of treatment with their healthcare providers.
How is stem cell therapy administered for MS?
Stem cell therapy for MS may be administered via various routes, including intravenous infusion, intrathecal injection, or direct transplantation into the central nervous system. Treatment protocols may vary depending on the type of stem cells used and the specific goals of therapy.
Is Stem Cell Therapy for MS Right For You?

In conclusion, stem cell treatments for multiple sclerosis (MS) represent a promising frontier in the field of regenerative medicine, offering hope for improved outcomes and quality of life for individuals living with this complex autoimmune disease.
While the evidence supporting the use of stem cell therapy for MS is still evolving, preliminary studies and clinical trials have shown encouraging results, suggesting the potential for modulating the immune response, promoting tissue repair, and restoring neurological function in MS patients.
However, it is important to acknowledge that stem cell therapy for MS is still in its early stages, and many questions remain regarding its safety, efficacy, and long-term outcomes. Challenges such as patient selection, optimal cell sources, treatment protocols, and standardization of outcomes assessments must be addressed through further research and clinical trials to maximize the therapeutic potential of stem cell treatments for MS.
Stem Cell Treatment Could Help Your Condition
Despite these challenges, the growing body of evidence supporting the use of stem cell therapy for MS underscores its potential as a transformative treatment approach for addressing the underlying disease processes and improving clinical outcomes in MS patients.
Continued research, collaboration, and investment in stem cell research hold the promise of advancing our understanding of MS pathophysiology and developing innovative therapies that offer hope for a brighter future for individuals affected by this debilitating disease.
If you or a loved one is interested in stem cell treatments and would like more information or would like to schedule a consultation, please reach out to us. We’re happy to help answer your questions about stem cell treatments for ms and if they may be right for you.