Mechanical arthritis, or osteoarthritis, affects millions by wearing down joint cartilage over time. Unlike inflammatory arthritis, it’s caused by physical stress on joints. In this article, we’ll cover its symptoms, causes, and available treatments, helping you navigate this challenging condition.
Key Takeaways
Mechanical arthritis, primarily identified as osteoarthritis, is a degenerative joint disease characterized by joint pain and stiffness due to cartilage wear, often influenced by mechanical stress.
Common symptoms include localized pain during movement, reduced mobility, and sensations of locking or catching in the joints, differentiating it from inflammatory forms of arthritis.
Treatment approaches for mechanical arthritis range from medications and physical therapy to surgical interventions, each tailored to individual needs and disease severity for effective management.
What is Mechanical Arthritis?
Mechanical arthritis, often synonymous with osteoarthritis, is a degenerative joint disease that primarily results from the wear and tear of joints over time. Unlike inflammatory arthritis, such as rheumatoid arthritis, mechanical arthritis is largely influenced by mechanical factors and mechanical stress on the joints. This condition leads to joint pain, stiffness, and eventual cartilage damage, significantly affecting the musculoskeletal system.
Osteoarthritis is driven by both mechanical and inflammatory factors, though the predominant influence is mechanical. The continuous wear on the cartilage that cushions the bones leads to its deterioration, causing the bones to rub against each other.
This friction results in arthritis pain and further joint damage. The interplay between mechanical forces, inflammatory cells, and inflammatory responses complicates the classification of osteoarthritis, fueling an ongoing debate among medical professionals.
The mechanical load on the joints, whether from regular activities or excessive strain, accelerates the degeneration process. Over time, this leads to a roughening and thinning of the cartilage, making every movement painful and difficult. Unlike inflammatory arthritis, which often affects joints symmetrically, mechanical arthritis usually targets one or two specific joints, often those that bear the most weight or have been previously injured, contributing to the inflammatory process.
Recognizing the role of mechanical forces in this degenerative joint disease is essential for effective treatment and management. Recognizing the impact of mechanical forces on joint damage is crucial for guiding preventive strategies and therapeutic interventions, ultimately enhancing the quality of life for those affected by mechanical arthritis.
Common Symptoms of Mechanical Arthritis
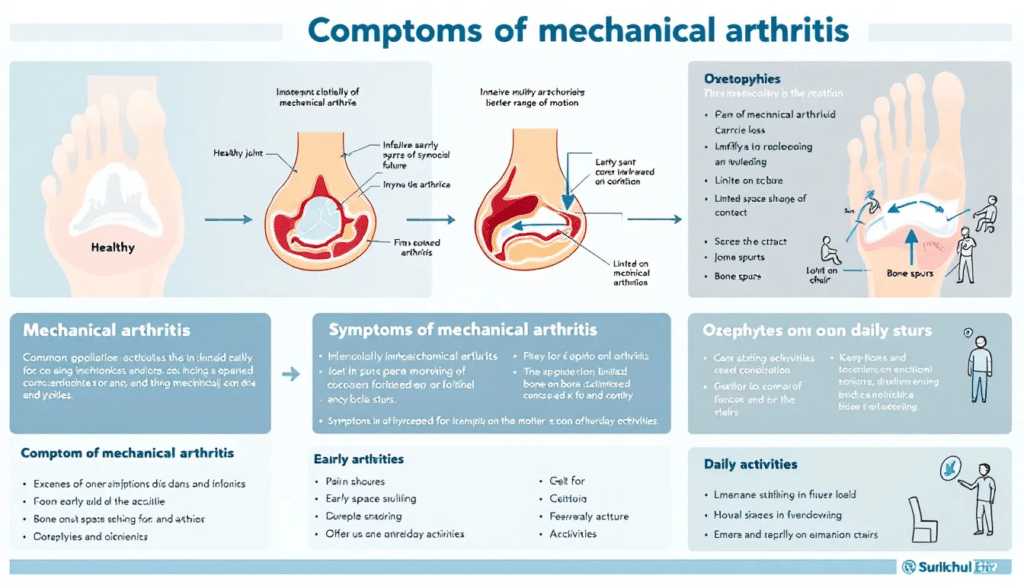
One of the most telling signs of mechanical arthritis is joint pain, which becomes more noticeable during movement and can be quite debilitating. This type of pain, often referred to as mechanical joint pain, tends to worsen after periods of activity and may be accompanied by stiffness. For those living with this condition, the pain can be a constant reminder of the wear their joints endure daily.
Mechanical joint pain is unique in its patterns. It typically worsens with use and improves with rest, unlike inflammatory arthritis, where pain can persist regardless of activity levels. This characteristic can help differentiate mechanical arthritis from other types of arthritis, such as rheumatoid arthritis. For many, the pain localizes to one or two joints, often the knee or hip, which bear the most mechanical load.
Reduced mobility is another hallmark of mechanical arthritis. As the cartilage wears away and the bones start to grind against each other, the range of motion in the affected joints diminishes. This limitation can make everyday tasks, such as walking or climbing stairs, increasingly challenging. The feeling of instability or weakness in the joint is another common symptom, further complicating mobility.
Other symptoms might include a sensation of the joints locking or catching during movement, which can be both painful and alarming. These symptoms, combined with the constant pain and stiffness, highlight the significant impact mechanical arthritis can have on one’s life. Recognizing these signs early is crucial for seeking appropriate treatment and managing the disease effectively.
Causes and Risk Factors
Aging is one of the most significant risk factors for mechanical arthritis. As we age, the wear and tear on our joints accumulate, making those over 55 particularly susceptible to this degenerative joint disease. However, aging is not the sole cause. Prior joint injuries or inflammation can also play a crucial role in the onset and progression of mechanical arthritis.
Mechanical arthritis often occurs when the mechanical demand on a joint exceeds its ability to maintain itself. This imbalance can stem from various factors, such as excessive mechanical stress, joint instability, or unfavorable biomechanical conditions like malalignment and loss of meniscal tissue. These conditions can lead to direct damage to the cartilage and subchondral bone, accelerating the degeneration process.
Joint instability, particularly in weight-bearing joints like the knees, can shift load-bearing areas, leading to uneven stress distribution and cartilage overloading. Over time, this can result in significant cartilage damage and joint degeneration. Additionally, the sensitivity of chondrocytes—the cells that produce cartilage—to mechanical loads means that extreme stress can accelerate cell aging and cartilage breakdown.
Certain health conditions, such as diabetes, can further elevate the risk of developing mechanical arthritis. These conditions can affect the body’s ability to repair joint tissues and manage inflammation, compounding the effects of mechanical stress. Understanding these risk factors is crucial for early intervention and prevention strategies, ultimately helping to mitigate the disease’s progression.
How Mechanical Forces Affect Joints
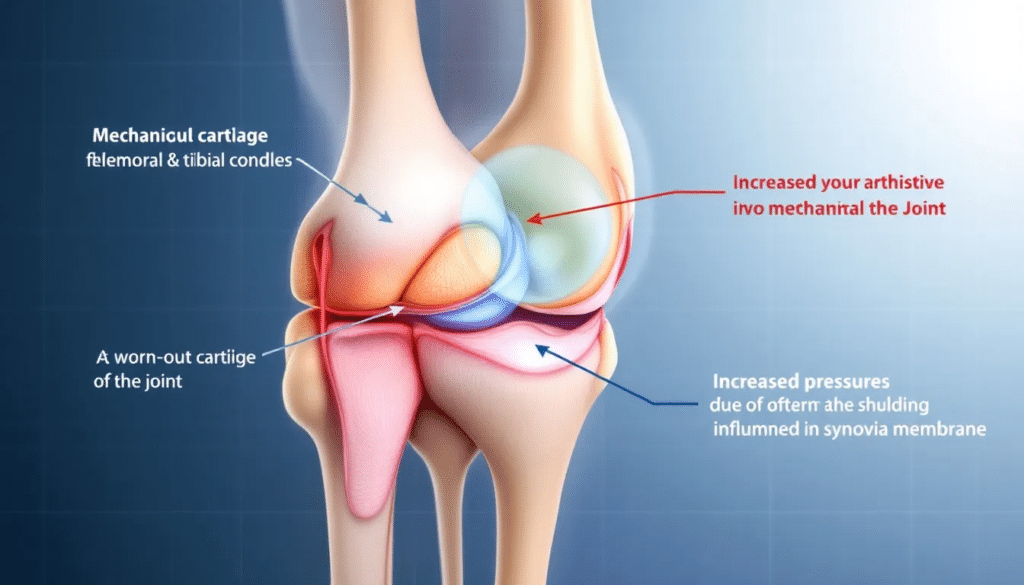
Mechanical arthritis primarily involves the deterioration of the cartilage that covers the ends of bones in joints. This cartilage acts as a cushion, facilitating smooth movement. When it wears down, the resulting friction causes the cartilage to become rough and thin, leading to significant joint pain and discomfort. This process is a key feature of osteoarthritis, a common type of mechanical arthritis.
As the cartilage continues to degrade, the bones start to remodel themselves in response to the increased stress. This remodeling can lead to the formation of osteophytes, or bony growths, which alter the shape of the joint and contribute to further pain and stiffness. Previous joint injuries can exacerbate this process, leading to long-term mechanical problems and increasing the likelihood of developing arthritis and disease progression.
The components that make up a joint affected by osteoarthritis include cartilage, synovium, subchondral bone, capsule, menisci, muscles, and tendons. Each of these components can be impacted by mechanical stress, leading to a complex interplay of damage and repair. The body’s primary response to mechanical injury in osteoarthritis is a pathophysiological attempt to correct abnormal mechanical stress, though this often leads to further joint damage.
Understanding how mechanical forces affect joints is crucial for developing effective treatment strategies. By addressing the underlying mechanical factors, we can better manage symptoms and slow the progression of this degenerative joint disease, ultimately improving the quality of life for those affected.
Diagnosis of Mechanical Arthritis
Diagnosing mechanical arthritis can be challenging, particularly in its early stages. Unlike inflammatory arthritis, such as rheumatoid arthritis, mechanical arthritis often arises from injuries sustained during sports or accidents. These injuries can lead to long-term mechanical problems that gradually wear down the joints.
One of the key diagnostic features of mechanical arthritis is the absence of inflammatory markers in conventional blood tests. This absence is a significant factor in distinguishing mechanical arthritis from other forms of arthritis, as conditions like rheumatoid arthritis typically show elevated inflammatory markers. Therefore, blood tests alone are often insufficient for a definitive diagnosis.
Imaging techniques play a crucial role in diagnosing mechanical arthritis. While x-rays and MRI scans are commonly used, they often don’t provide much help in the early stages of the disease. However, techniques like MRI with contrast and ultrasonography are considered valid for studying synovitis in osteoarthritis, offering more detailed insights into the condition. These imaging techniques can reveal the extent of joint damage and help guide treatment decisions.
Differentiating mechanical arthritis from other forms of arthritis is essential for effective treatment. By understanding the unique diagnostic features of this condition, healthcare providers can develop targeted treatment plans that address the specific needs of those affected by mechanical arthritis.
Treatment Options for Mechanical Arthritis
Managing mechanical arthritis requires a multifaceted approach to alleviate pain and improve joint function. Treatment options range from medications and physical therapy to surgical interventions, each tailored to the severity of the condition and individual patient needs.
Medications, such as NSAIDs (Non-Steroidal Anti-Inflammatory Drugs), are often the first line of treatment for managing arthritis pain and reducing inflammation. Physical therapy plays a critical role in enhancing joint mobility and decreasing pain through targeted exercises and manual therapies. For severe cases where conservative treatments no longer provide relief, surgical interventions like joint replacement or arthroscopy may be considered.
Each of these treatment options has its own set of benefits and considerations. Medications can provide quick relief but may have side effects. Physical therapy requires commitment and consistency but can significantly improve joint function without the need for surgery. Surgical interventions offer a more permanent solution but come with their own risks and recovery times.
Understanding these treatment options and their potential impacts is crucial for making informed decisions about managing mechanical arthritis. By exploring each option in detail, we can better navigate the journey toward improved joint health and quality of life.
Medications
Medications play a crucial role in managing the pain and inflammation associated with mechanical arthritis. Non-steroidal anti-inflammatory drugs (NSAIDs) are commonly used as initial non-surgical treatments for this condition. These medications work by reducing inflammation and alleviating pain, providing much-needed relief for those suffering from arthritis pain.
Commonly prescribed NSAIDs include ibuprofen and naproxen, which can help manage the symptoms of mechanical arthritis effectively. Analgesics, another class of pain relievers, are also frequently used. These medications target the pain directly, making daily activities more manageable for patients.
While medications can provide significant relief, they are not without potential side effects. Long-term use of NSAIDs can lead to gastrointestinal issues, cardiovascular problems, and other health concerns. Using these medications under the guidance of a healthcare provider helps minimize risks.
For many, medications are a critical component of a comprehensive treatment plan for mechanical arthritis. When used appropriately, they can significantly improve the quality of life, allowing individuals to manage their symptoms and maintain their daily routines more effectively.
Physical Therapy
Physical therapy is recognized as one of the most effective non-drug treatments for mechanical arthritis. It focuses on tailored exercises and manual techniques designed to enhance joint function and reduce pain. Strengthening the muscles around the joints through physical therapy improves stability and mobility, making daily activities less painful and more manageable.
Therapeutic exercises are a cornerstone of physical therapy for mechanical arthritis. These exercises are carefully designed to stretch and strengthen the muscles supporting the joints, thereby reducing the mechanical load on the affected areas. Regular physical therapy sessions can lead to significant improvements in joint function and a reduction in arthritis pain.
Manual therapy techniques, such as massage and joint mobilization, are also used to alleviate pain and improve physical function. These techniques can help reduce inflammation and stiffness, providing immediate relief and long-term benefits.
The combination of tailored exercises and manual therapies makes physical therapy a highly effective treatment option for mechanical arthritis. By committing to a regular physical therapy routine, individuals can significantly enhance their joint health and overall quality of life.
Surgical Interventions
For severe cases of mechanical arthritis where conservative treatments fail to provide relief, surgical interventions may be necessary. These procedures aim to repair or replace damaged joints, thereby relieving pain and restoring function.
Joint replacement surgery is one of the most common surgical options for advanced mechanical arthritis. This procedure involves replacing the damaged joint with an artificial one, significantly reducing pain and improving mobility. While it is highly effective, joint replacement surgery requires a significant recovery period and carries risks associated with any major surgery.
Arthroscopy is a minimally invasive surgical procedure that can be used to diagnose and treat joint issues related to mechanical arthritis. During an arthroscopy, a small camera is inserted into the joint, allowing the surgeon to see and repair damaged tissues. This procedure is less invasive than joint replacement and often results in quicker recovery times.
While surgical interventions can provide significant relief, they are typically considered only when other treatments have failed. Understanding the risks and benefits of these procedures is crucial for making informed decisions about managing severe mechanical arthritis.
Preventing Further Joint Damage
Preventing further joint damage is a crucial aspect of managing mechanical arthritis. One of the most effective strategies is maintaining a healthy weight, as obesity significantly increases stress on the joints, particularly in weight-bearing areas like the knees and hips. Losing weight can reduce this stress, slowing the progression of joint damage.
Incorporating low-impact exercises, such as swimming and cycling, into your routine can provide cardiovascular benefits while minimizing joint stress. These activities help maintain joint mobility and overall fitness without exacerbating arthritis pain. Regular hydration is also essential for joint health, as it helps maintain joint lubrication and reduces stiffness.
Implementing joint protection strategies, such as using the strongest joints for tasks, can help minimize discomfort and prevent further joint damage. Practicing good ergonomics in the workplace, such as using an ergonomic chair and proper desk setup, can prevent joint strain. Wearing supportive footwear that provides arch support and shock absorption can also help reduce joint strain.
Using assistive devices like splints and lever arm tools can provide additional support for weakened joints and reduce the force needed to perform daily tasks. These strategies, combined with a healthy lifestyle, can significantly reduce the risk of further joint damage and improve the quality of life for those living with mechanical arthritis.
Living with Mechanical Arthritis

Living with mechanical arthritis often means adapting to new ways of performing everyday tasks to minimize pain and prevent further joint damage. Regular breaks during activities can prevent fatigue and joint strain, enhancing overall performance in daily tasks. This simple adjustment can make a significant difference in managing the symptoms of mechanical arthritis.
Lever arm devices, such as door handles and jar openers, are invaluable tools for reducing the amount of force needed when performing tasks, thus minimizing stress on smaller joints. Similarly, using larger, rounded handles on tools makes gripping easier and lessens the fatigue experienced in arthritic hands. These modifications can make daily tasks more manageable and less painful.
In advanced cases of mechanical arthritis, visible deformities of the joint may develop, making daily activities even more challenging. Swelling around the affected joint can also occur due to fluid accumulation, adding to the discomfort. Managing these symptoms often requires a combination of medical treatments and lifestyle adjustments.
Despite these challenges, many people with mechanical arthritis find ways to maintain a high quality of life. Incorporating practical strategies and staying proactive about joint health enables continued engagement in enjoyable activities and helps maintain independence.
Summary
Mechanical arthritis, a condition that affects millions worldwide, is more than just a consequence of aging. Understanding its symptoms, causes, and treatment options is crucial for managing this degenerative joint disease. From recognizing the early signs of joint pain and stiffness to exploring effective treatments like medications, physical therapy, and surgical interventions, knowledge is a powerful tool.
Preventing further joint damage through weight management, low-impact exercises, and ergonomic practices can make a significant difference in the progression of mechanical arthritis. Living with this condition requires a proactive approach, incorporating both medical treatments and lifestyle adjustments to maintain mobility and reduce pain.
By staying informed and engaged in their treatment plans, individuals with mechanical arthritis can improve their quality of life and continue to enjoy their daily activities. Embracing these strategies can help manage symptoms and prevent the condition from taking over their lives.
Frequently Asked Questions
What is the difference between mechanical and inflammatory arthritis?
The primary distinction between mechanical and inflammatory arthritis lies in their causes; mechanical arthritis results from wear and tear on the joints, while inflammatory arthritis is driven by an autoimmune response that prompts joint inflammation. Understanding this difference is crucial for effective management and treatment approaches.
What are the common symptoms of mechanical arthritis?
The common symptoms of mechanical arthritis include joint pain that intensifies with activity, stiffness, reduced mobility, instability in the joint, and potential swelling or deformities in advanced stages. It is essential to monitor these symptoms for appropriate management.
How can mechanical arthritis be diagnosed?
Mechanical arthritis is diagnosed through a combination of patient history, physical examinations, and imaging techniques such as MRI and x-rays, alongside blood tests to rule out inflammatory markers. This comprehensive approach ensures accurate identification of the condition.
What treatment options are available for mechanical arthritis?
For mechanical arthritis, effective treatment options comprise nonsteroidal anti-inflammatory drugs (NSAIDs) for pain relief, physical therapy to enhance joint function, and, in severe cases, surgical interventions such as joint replacement or arthroscopy.
How can I prevent further joint damage if I have mechanical arthritis?
To prevent further joint damage from mechanical arthritis, it is essential to maintain a healthy weight, engage in low-impact exercises, and employ joint protection strategies. Additionally, practicing good ergonomics and wearing supportive footwear can significantly reduce strain on your joints.