The intricate workings of the human body heavily depend on the optimal function of various components, with cartilage standing out as a critical player. Serving as specialized connective tissue, cartilage is instrumental in providing joint cushioning, facilitating smooth movement, and maintaining structural integrity.
Unfortunately, the regenerative capabilities of cartilage are limited, making it susceptible to wear and tear, osteoarthritis, and injuries. In the realm of regenerative medicine, the utilization of stem cells has emerged as a beacon of hope.
The central question that emerges is: Can stem cells regrow cartilage? This exploration into regenerative medicine delves into the dynamic intersection of state-of-the-art stem cell research and the urgent need for effective solutions to address cartilage-related issues. It seeks to unravel the promises, hurdles, and potential breakthroughs that could revolutionize medical interventions for cartilage regeneration.
Can Stem Cells Regrow Cartilage?

Yes, stem cells have shown promise in regrowing cartilage. Stem cell therapy research indicates that certain types of stem cells can differentiate into cartilage cells and contribute to tissue regeneration. Stem cell therapy regenerative medicine may assist in cartilage repair in cases of damaged cartilage.
Stem cell-based therapies are being explored as potential treatments for cartilage damage, offering hope for improved outcomes in conditions like osteoarthritis and injuries affecting joint health. However, challenges and further research are still needed to optimize these treatments for widespread clinical use.
The researchers used powerful molecules called bone morphogenetic protein 2 (BMP2) to initiate bone formation after microfracture. However, they then stopped the process midway with a molecule that blocked another signaling molecule important in bone formation, called vascular endothelial growth factor (VEGF).
Working in a mouse model test, the research team documented that microfractures did, in fact, activate skeletal stem cells to begin working on repair. CXCR4 transfection of cord blood mesenchymal stromal cells with the use of cationic liposome enhances their migration toward stromal cell form. Early results show that bone marrow aspirate concentrate is safe to use and is a reliable and viable (stem cell) cellular product.
Explanation of common cartilage-related issues and their impact on health

Cartilage-related issues pose significant challenges to overall health and well-being, given the pivotal role cartilage plays in supporting the body’s structure and function. These issues encompass a range of conditions with distinct impacts:
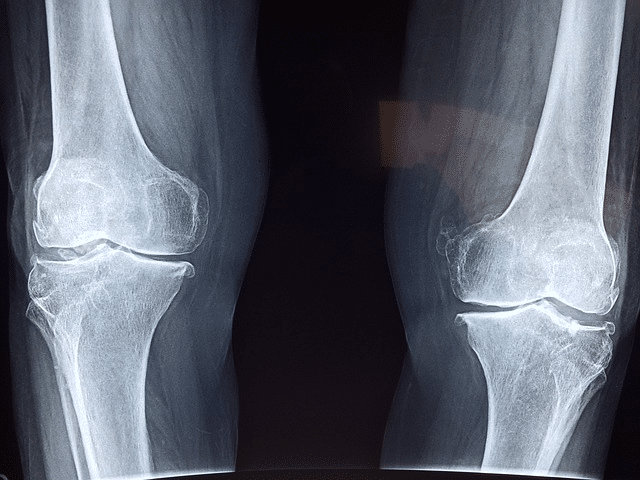
Osteoarthritis (OA): This degenerative joint disease results in the breakdown of cartilage covering bone ends within joints. As cartilage deteriorates, bones can grind against each other, causing stiffness, pain, and diminished joint mobility. OA commonly affects weight-bearing joints like the knees, hips, and spine.
Traumatic Injuries: Accidents, sports-related incidents, or trauma can inflict damage on cartilage, leading to tears, fractures, or dislocations. Such damage disrupts the smooth cartilage surface, resulting in pain, swelling, and potential long-term joint complications.
Rheumatoid Arthritis (RA): An autoimmune disorder, RA primarily targets the synovium – the membranes surrounding joints. Inflammation triggered by RA can harm cartilage and adjacent structures, contributing to joint deformities, pain, and functional limitations.
Cartilage Defects and Lesions: Conditions like chondromalacia or focal cartilage defects involve localized damage or softening of cartilage in specific joint areas. These defects can manifest as pain, compromised joint stability, and restricted movement.
Degenerative Disc Disease: The intervertebral discs in the spine, composed of cartilage, may undergo degeneration. Degenerative disc disease results in pain, reduced spinal flexibility, and nerve compression, impacting overall back health.
Avascular Necrosis: This condition arises from bone tissue death due to insufficient blood supply. When joints are affected, avascular necrosis can lead to bone collapse, compromising joint stability and causing cartilage damage.
The repercussions of these cartilage-related issues on health vary from localized joint discomfort to broader effects on mobility, physical function, and even psychological well-being. Chronic cartilage problems may curtail daily activities, limit exercise capacity, and contribute to a diminished quality of life.
Management strategies typically involve pain relief, physical therapy, and, in severe cases, surgical interventions like joint replacement or cartilage repair procedures. Regenerative medicine options like stem cell therapy are also emerging as options for cartilage repair.
Types of cartilage in the human body
The human body contains three primary types of cartilage, each with distinct structural characteristics and functions:
Hyaline Cartilage
Hyaline cartilage is characterized by its smooth and glassy appearance, primarily due to a high concentration of collagen fibers. This type of cartilage is found in areas requiring smooth joint movement and flexibility, serving as a cushion in joints to reduce friction. Examples of its location include the nose, trachea, larynx, and the ends of long bones.
Elastic Cartilage
Elastic cartilage contains a higher proportion of elastic fibers in addition to collagen fibers. This structural composition provides greater flexibility. Elastic cartilage is commonly found in regions where flexibility and elasticity are essential, such as the external ear, epiglottis, and certain parts of the larynx.
Fibrocartilage
Fibrocartilage is distinguished by its dense collagen fibers, imparting strength and durability. This type of cartilage acts as a shock absorber and provides support in areas requiring strength. Fibrocartilage is present in structures like intervertebral discs, pubic symphysis, and certain tendons, including the knee meniscus. Stem cell therapy may help with knee pain by repairing knee cartilage.
Common Causes of Cartilage Damage

Osteoarthritis, a degenerative joint disease, manifests as the gradual breakdown of articular cartilage. The wear and tear on cartilage over time leads to diminished joint cushioning, resulting in pain, stiffness, and reduced mobility. Traumatic injuries, such as accidents, sports injuries, or direct trauma, can cause immediate damage to cartilage.
Tissue Repair After Damage to Healthy Cartilage
Tears, fractures, or dislocations can disrupt the smooth surface of articular cartilage, causing pain, swelling, and potential long-term joint issues. In the context of cartilage repair, mesenchymal stem cells, particularly autologous mesenchymal stem cells derived from the bone marrow, play a crucial role in the body’s natural healing processes. Rheumatoid arthritis (RA), an autoimmune disorder, can affect the synovium, leading to inflammation and cartilage damage.
Inflammatory processes contribute to joint deformities, pain, and functional limitations as cartilage is compromised. Overuse and repetitive strain involve continuous stress or strain on specific joints due to repetitive activities, contributing to cartilage wear. Over time, this can lead to cartilage degeneration and conditions like chondromalacia.
Aging is a natural process contributing to a gradual decline in the quality and quantity of articular cartilage. Reduced cartilage elasticity and increased susceptibility to damage can occur, making joints more prone to issues like osteoarthritis.
Genetics & Articular Cartilage Defects

Genetic factors may predispose some individuals to cartilage-related conditions, influencing the structural integrity of articular cartilage and potentially increasing the risk of conditions such as osteoarthritis. Avascular necrosis results from a lack of blood supply to bone and surrounding tissues. When this affects joints, it can lead to bone collapse and subsequent damage to articular cartilage due to compromised blood flow.
Meniscus tears can occur due to sudden twisting or trauma, leading to disruptions in the fibrocartilage in the knee joint. Mesenchymal stem cell therapy holds promise for naturally promoting cartilage repair, utilizing the regenerative potential of adult stem cells to maintain healthy cartilage.
How stem cells can differentiate into cartilage cells
According to many studies, stem cells possess the remarkable ability to differentiate themselves into various cell types, including cartilage cells, through a process known as chondrogenesis. This differentiation occurs in response to specific signaling pathways and environmental cues. Here’s an overview of how stem cells can differentiate into cartilage cells:
Pluripotent Stem Cells
Pluripotent stem cells, such as embryonic stem cells (ESCs) and induced pluripotent stem cells (iPSCs), have the potential to differentiate into cells of all three germ layers, including mesoderm-derived cells like chondrocytes (cartilage cells).
Mesenchymal Stem Cells (MSCs)
MSC Mesenchymal Stem Cells are adult stem cells found in various forms of tissues, including bone marrow, adipose tissue, and umbilical cord blood. They are multipotent cells, meaning they can differentiate into several cell types, including chondrocytes.
Chondrogenic Induction
To induce chondrogenesis, stem cells are exposed to specific growth factors and signaling molecules. Transforming Growth Factor-beta (TGF-β) is a key signaling factor known for its role in promoting chondrogenesis.
Formation of Micromass Cultures
In laboratory settings, stem cells can be aggregated into micro mass cultures, creating three-dimensional environments that mimic the conditions conducive to cartilage formation.
Expression of Chondrogenic Markers
During chondrogenesis, the stem cells undergo changes in gene expression, leading to the activation of chondrogenic markers. Important markers include collagen type II, aggrecan, and Sox9, which are characteristic of mature cartilage cells.
Extracellular Matrix Production
As differentiation progresses, the cells start synthesizing and depositing the extracellular matrix (ECM) components typical of cartilage, such as collagen and proteoglycans. This matrix provides structural support to the developing cartilage tissue.
Maturation and Maintenance
The newly formed cartilage cells, or chondrocytes, mature and organize into functional tissue structures. The process is finely regulated to ensure the proper development and maintenance of cartilage.
Understanding the molecular mechanisms and signaling pathways involved in chondrogenesis is crucial for optimizing stem cell-based therapies for cartilage repair. Researchers aim to harness the regenerative potential of stem cells to develop effective treatments for conditions such as osteoarthritis and injuries that affect the cartilage in joints.
How do stem cells work to regrow cartilage?

Stem cells contribute to the regrowth of cartilage through their unique ability to differentiate into chondrocytes, the specialized cells responsible for cartilage formation and maintenance. The process of how stem cells work to regrow cartilage involves several key steps:
Chondrogenic Induction
Stem cells are exposed to specific signaling molecules and growth factors that promote chondrogenesis, the process of differentiation into chondrocytes. Transforming Growth Factor-beta (TGF-β) is a crucial signaling factor in this context.
Stem Cell Activation and Differentiation
The exposure to chondrogenic factors activates certain genes in the stem cells, initiating a cascade of molecular events that drive their differentiation into chondrocytes. These cells acquire the characteristics and functions of cartilage cells.
Formation of Cartilage Tissue
The differentiated stem cells, now functioning as chondrocytes, start producing the extracellular matrix (ECM) components specific to cartilage, such as collagen and proteoglycans. The ECM provides structural support and elasticity to the developing cartilage tissue.
Three-Dimensional Cultures
In some regenerative approaches, stem cells are cultured in three-dimensional environments, mimicking the natural conditions conducive to cartilage formation. This approach allows the cells to organize and interact more naturally, promoting the development of functional cartilage tissue.
Implantation or Injection
The generated cartilage-like tissue can be implanted or injected into the damaged area, depending on the specific therapeutic approach. This can be done through surgical procedures or minimally invasive techniques.
Integration with Existing Cartilage
The transplanted or injected cartilage-like tissue integrates with the existing cartilage, promoting structural integrity and enhancing the overall function of the joint.
Securing Long-Term Viability
Ensuring the long-term viability of the regenerated cartilage is a critical aspect. Researchers explore various strategies to enhance cell survival, integration, and functionality over time.
Monitoring and Follow-Up
Post-treatment, monitoring the patient’s response and the quality of regenerated cartilage is essential. Follow-up assessments may include imaging studies, such as MRI, and clinical evaluations to track improvements and address any ongoing concerns.
By harnessing the regenerative potential of stem cells and guiding their differentiation into chondrocytes, researchers and clinicians aim to develop effective treatments for cartilage-related conditions, including osteoarthritis and injuries affecting joint health. This approach holds promise for enhancing the body’s natural ability to repair and regenerate damaged cartilage.
Future Directions and Challenges of Addressing Cartilage Defects
This section of the article delves into the potential avenues for advancement in stem cell research for cartilage regeneration, while also addressing the obstacles and areas that require further exploration. Here’s an in-depth exploration:
Emerging Technologies and Techniques in Stem Cell Research for Cartilage Regeneration
Advanced Biomaterials: Explore the integration of advanced biomaterials to enhance the delivery and retention of stem cells in target areas. Developments in biomaterial science can provide scaffolds that mimic the natural cartilage environment, fostering improved regeneration.
3D Printing: Investigate the use of 3D printing technology to create intricate structures that support the growth of cartilage tissue. Precision in spatial arrangement and composition could be critical for generating functional and anatomically accurate cartilage.
CRISPR/Cas9 Technology: Explore the potential of gene-editing technologies like CRISPR/Cas9 to modify and enhance the therapeutic properties of stem cells. This may involve optimizing the expression of genes associated with chondrogenesis for more effective cartilage regeneration.
Potential Obstacles and Areas for Improvement in Stem Cell-Based Therapies
Incomplete Integration: Address challenges related to the complete integration of regenerated cartilage with the surrounding tissue. Achieving seamless integration is crucial for restoring normal joint function and preventing further complications.
Long-Term Viability: Investigate strategies to improve the long-term viability of transplanted or generated cartilage tissue. Ensuring sustained functionality and resilience over time is a key aspect of successful stem cell-based therapies.
Immunological Rejection: Develop approaches to mitigate potential immunological responses to transplanted cells. Strategies may include refining the selection of cell sources, optimizing immunosuppressive protocols, or exploring immune-tolerant stem cell lines.
Collaborative Efforts Between Researchers, Clinicians, and Policymakers to Advance the Field
Interdisciplinary Collaboration: Emphasize the need for interdisciplinary collaboration between researchers, clinicians, and policymakers. This collaborative approach can facilitate the translation of research findings into clinical applications, ensuring that advancements reach patients effectively.
Standardization and Regulation: Advocate for standardized protocols and regulatory frameworks governing stem cell-based therapies. Establishing clear guidelines can enhance the safety, efficacy, and ethical standards of these treatments, fostering public trust and regulatory approval.
Patient-Specific Approaches: Explore personalized or patient-specific approaches in stem cell therapy. Tailoring treatments to individual patient characteristics, including genetic factors and the specific nature of cartilage damage, may enhance treatment outcomes.
Cartilage Injury & Cartilage Growth Frequently Asked Questions

What is the role of cartilage in the human body?
Cartilage provides structural support to joints, facilitates smooth movement, and acts as a cushion between bones, preventing friction and damage.
Can stem cells naturally regrow cartilage in the body?
Yes, stem cells have the potential to differentiate into cartilage cells through a process called chondrogenesis, contributing to the regrowth of cartilage.
What types of stem cells are involved in cartilage regeneration?
Pluripotent stem cells (such as embryonic stem cells), multipotent adult stem cells, and induced pluripotent stem cells (iPSCs) are all explored for their ability to differentiate into cartilage cells.
How do stem cells differentiate into cartilage cells?
Stem cells can undergo chondrogenesis, a process where they are exposed to specific growth factors and signaling molecules that guide their differentiation into chondrocytes, the cells responsible for cartilage formation.
How are stem cells delivered for cartilage regeneration?
Stem cells can be delivered through injection, implantation, or as part of three-dimensional cultures. The method depends on the specific therapeutic approach and the nature of the cartilage damage.
Can Stem Cells Regrow Cartilage After Cartilage Defects Emerge?

The exploration of stem cells regrowing cartilage offers hope for treating conditions like osteoarthritis and traumatic injuries. Stem cells, sourced from various origins, show promise in differentiating into cartilage cells through chondrogenesis.
While advancements are evident, challenges include seamless integration of regenerated cartilage, addressing long-term viability, and managing potential immunological responses. Ethical considerations and regulatory frameworks highlight the need for careful navigation in translating these advancements into clinical settings.
Successful cases and ongoing trials underscore the potential efficacy of stem cell-based treatments. Collaborative efforts between researchers, clinicians, and policymakers are crucial for overcoming challenges and establishing standardized protocols. The future of stem cell research in cartilage regeneration holds promise, with emerging technologies like 3D printing and gene-editing enhancing possibilities.
The focus is not only on scientific inquiry but also on transforming lives by providing relief, improved mobility, and a better quality of life. Continued research, interdisciplinary collaboration, and ethical practices are essential to redefine orthopedic medicine through the regenerative power of stem cells. The journey from the laboratory to clinical applications is underway, signaling a potential transformation in musculoskeletal healthcare.
Book An Appointment With Stem Cells LA

Are you or someone you know dealing with the challenges of cartilage damage, such as osteoarthritis or joint injuries? Wondering can stem cells regrow cartilage you or a loved one damaged or lost from injury? Discover the potential of stem cell therapy in regrowing cartilage and rejuvenating joint health.
If you’re seeking alternatives to conventional treatments or are interested in the transformative possibilities of stem cells, reach out to Stem Cells LA for a personalized consultation. Take the first step toward a future with improved joint function and reduced pain through the regenerative power of stem cells.
Contact Information:
???? Call or Text: 310-281-6160
???? Visit Us:
1970 S. Prospect Ave. Suite 2
Redondo Beach, CA 90277


