Can stem cells treat back pain? For those suffering from chronic back issues, stem cell therapy offers hope. This article will explain how stem cells to treat back pain work, what the process involves, and what outcomes you can expect.
Key Takeaways
Mesenchymal stem cells (MSCs) are key in treating back pain due to their unique ability to restore damaged tissues and promote long-term healing.
Different methods for administering stem cell therapy, including intradiscal injections and intravenous infusions, offer targeted or systemic approaches to alleviate back pain.
Patient eligibility and thorough screening are crucial to ensure safety and maximize the effectiveness of stem cell therapies for back pain.
Understanding Stem Cells and Their Role
Stem cells are extraordinary undifferentiated cells. They have the ability to develop into specialized cells and can also self-renew.
They play a crucial role in tissue maintenance and repair following an injury, acting as a natural repair system within the human body.
Various types of stem cells exist, including:
Embryonic stem cells, which can differentiate into almost any human cell
Adult stem cells, which have a more limited range of differentiation
Induced pluripotent stem cells (iPSCs), which are adult cells reprogrammed to behave like embryonic stem cells, providing another versatile source for regenerative therapies.
Among these, mesenchymal stem cells (MSCs) are particularly noteworthy due to their ability to rebuild damaged tissues. MSCs act as an internal repair system, making them invaluable in regenerative medicine. Grasping the fundamental nature of stem cells allows for a deeper appreciation of their potential in treating back pain and other degenerative conditions.
Mesenchymal Stem Cells for Back Pain
Mesenchymal stem cells (MSCs) have emerged as a powerful tool in the fight against back pain. These stem cells, derived from various tissues, are known for their unique ability to restore injured tissues, making them ideal for treating conditions like degenerative disc disease. Stem cell therapy for back pain primarily harnesses MSCs’ natural repair processes to heal deteriorated spinal discs.
One of the remarkable features of MSCs is their ability to differentiate into specialized cells essential for regenerating damaged intervertebral discs. This means that MSCs can not only relieve pain but also promote the long-term repair of the affected areas. Additionally, MSCs secrete various growth factors that stimulate tissue repair and decrease inflammation. This dual benefit of reducing inflammation while promoting healing makes MSCs particularly effective for patients suffering from chronic back pain.
Moreover, MSCs possess potent anti-inflammatory properties that can help reduce pain and promote faster healing. Modulating the immune response and suppressing inflammation, MSCs foster a favorable environment for tissue regeneration. This holistic approach to healing ensures that patients experience not only immediate pain relief but also long-lasting improvements in their condition.
Sources of Mesenchymal Stem Cells
Mesenchymal stem cells (MSCs) can be sourced from various tissues, each with its own set of advantages and limitations. One common source is bone marrow, where bone marrow stem cells have been extensively used in clinical applications. However, this method may have limitations due to patient age and health.
Adipose tissue, or fat, is another plentiful source of MSCs. These stem cells are often harvested because of their ample availability and ease of extraction.
Additionally, different compartments of the umbilical cord, such as Wharton’s jelly and perivascular regions, can provide MSCs. The collection of umbilical cord tissue-derived MSCs (CT-MSCs) is ethically acceptable, less invasive, and demonstrates superior immunomodulatory properties compared to bone marrow-derived MSCs.
Access to various sources ensures a versatile and effective approach to stem cell therapy.
Degenerative Disc Disease and Stem Cell Therapy
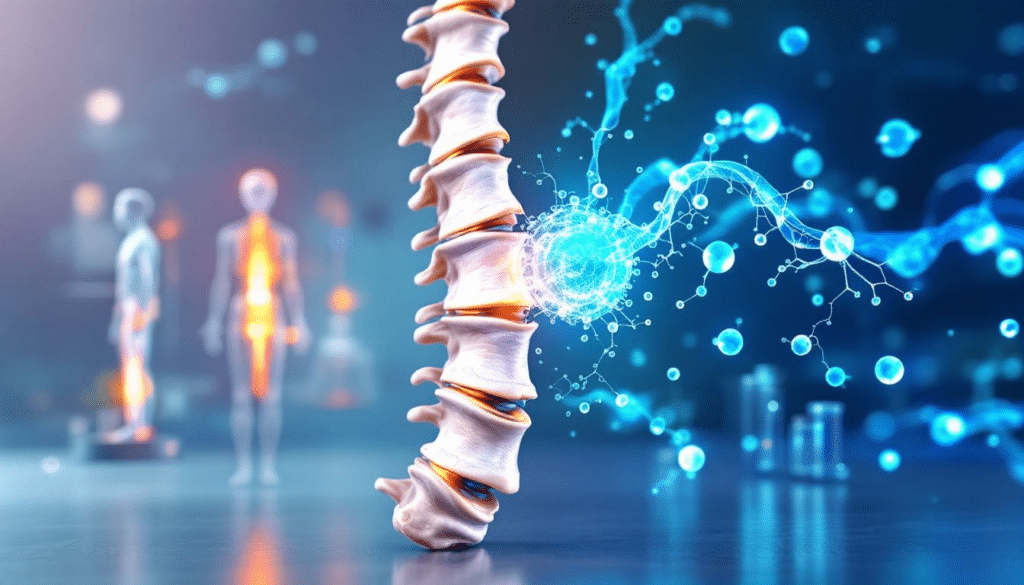
Degenerative disc disease is a common culprit behind chronic back pain, but stem cell therapy offers a promising solution. The goal of stem cell therapy is to regenerate damaged tissues using stem cells, effectively repairing intervertebral discs and alleviating pain. Intradiscal stem cell injections, which involve extracting stem cells from the patient’s bone marrow and injecting them into damaged discs, have shown considerable promise in promoting healing.
Mesenchymal stem cell (MSC) injections not only alleviate pain but also encourage the damaged intervertebral discs to repair themselves. These cells can differentiate into various specialized cells, promoting the structural integrity of the discs. This regeneration process is vital for restoring the disc’s function and providing long-term relief to patients suffering from degenerative disc disease.
Furthermore, MSC therapy aids in the repair and regeneration of injured tissues by differentiating into disc-like cells that restore the disc’s structural integrity. Actively contributing to tissue repair, MSCs provide a holistic approach to treating chronic back pain and disc degeneration.
Administration Methods for Stem Cell Treatments
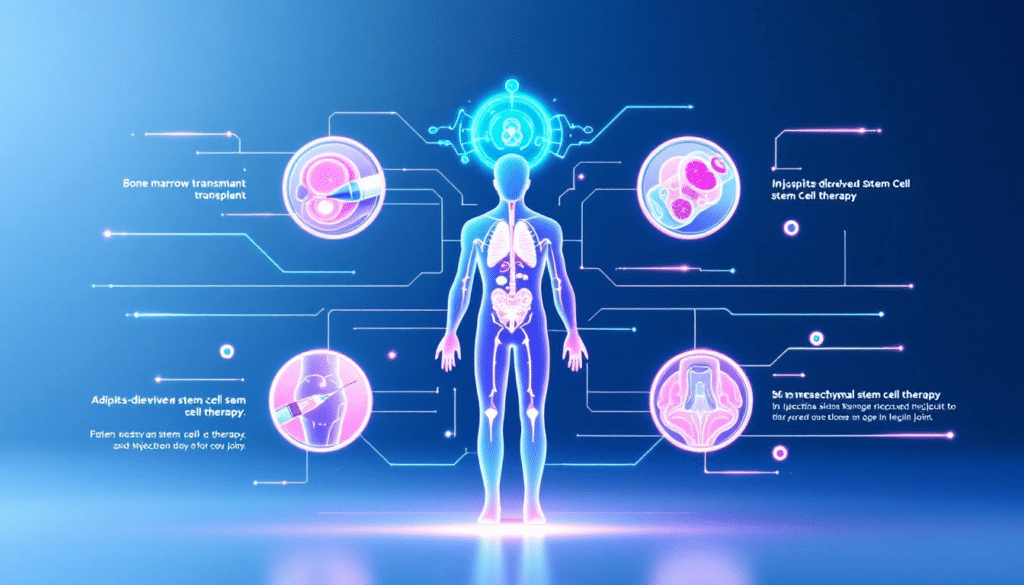
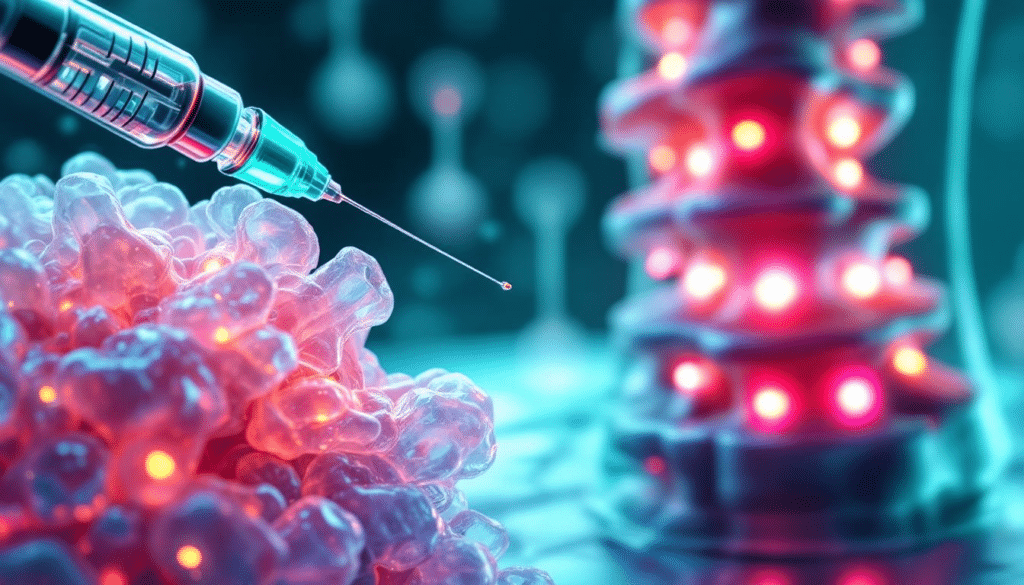
Administering stem cell treatments effectively is crucial for their success. One method is intradiscal injections, which specifically target spinal discs and require imaging guidance, such as fluoroscopy, to ensure accurate placement. This method is particularly effective for conditions like degenerative disc disease, as it delivers stem cells directly to the site of degeneration.
Another method is intravenous (IV) delivery, where stem cells are administered through the bloodstream. This approach allows stem cells to circulate and reach areas of inflammation through a process known as homing. IV delivery is minimally invasive and can reduce recovery time and postoperative complications compared to traditional surgeries.
Familiarity with these methods aids in selecting the most suitable treatment for each case.
Intradiscal Stem Cell Injections
Intradiscal stem cell injections are a targeted approach to treating back pain. The purpose of these injections is to repair damaged disc tissue. They also work to restore disc height and alleviate pain. Conditions such as degenerative disc disease and herniated discs can benefit significantly from this method.
Research has shown that stem cell implantation in animal models can enhance disc hydration and increase disc height, demonstrating the potential for significant improvements in human patients. Stem cells also secrete bioactive factors that positively influence the healing process in damaged discs. This targeted approach ensures higher local concentrations of stem cells, maximizing their regenerative potential.
Intravenous Stem Cell Infusions
Intravenous (IV) delivery of mesenchymal stem cells (MSCs) offers a systemic approach to treating back pain. This method is minimally invasive and allows for the widespread distribution of stem cells throughout the body. IV delivery is particularly beneficial for addressing multiple areas of inflammation and degeneration.
Cord tissue-derived mesenchymal stem cells (CT-MSCs) used in IV infusions provide superior immunomodulatory properties and faster self-renewal capabilities. Moreover, the higher bioavailability of intravenously administered MSCs leads to better pain relief and improved tissue regeneration.
While there are potential risks such as infection and allergic reactions, clinical trials have shown promising results with significant improvements in pain relief and function.
Comparing Injection and Infusion Methods
When it comes to delivering mesenchymal stem cells for back pain treatment, both intradiscal injections and intravenous infusions have their merits. Intradiscal injections deliver stem cells directly to the intervertebral disc, ensuring higher local concentrations and targeting the site of degeneration more effectively.
On the other hand, intravenous infusions are less invasive and can address multiple areas of inflammation simultaneously. Patient preference may vary, with some favoring the lower discomfort associated with IV infusions. However, intradiscal injections usually require imaging guidance for accuracy, adding to the complexity of the procedure.
Recognizing these differences aids in making an informed decision about the best treatment method.
Supportive Therapies to Enhance Stem Cell Treatment
Supportive therapies play a crucial role in optimizing the effectiveness of stem cell treatments for spine damage. Physiotherapy, for instance, focuses on improving movement and recovery through personalized treatment plans involving exercises and education.
Shockwave therapy utilizes high-energy sound waves to induce microtraumas, promoting healing and regeneration. Additionally, intravenous nutrition delivers essential nutrients directly into the bloodstream, bypassing digestive limitations and enhancing overall health post-treatment.
The dual approach of combining these supportive therapies with stem cell treatments can significantly enhance recovery and outcomes for patients.
Clinical Trials and Success Rates
The clinical application of stem cell therapy for degenerative disc disease is still in its early stages, with many trials ongoing. The Mayo Clinic, for example, is conducting multiple clinical trials to evaluate the safety and effectiveness of mesenchymal stem cells for treating low back pain.
Preliminary evidence suggests potential benefits of biologic treatments, including stem cells, for discogenic low back pain, though the overall evidence quality is currently low. Despite this, studies indicate that stem cell injections can lead to long-lasting pain relief and functional improvement in patients.
Additional studies are essential to determine the long-term effectiveness of these treatments. Their safety also requires further investigation.
Risks and Considerations
While stem cell therapy for back pain holds promise, it is important to be aware of the potential risks and considerations. Currently, these therapies are not FDA-approved, raising concerns about unregulated procedures that patients may encounter. Potential side effects from stem cell injections include nausea, vomiting, and infections at the injection site.
Intravenous stem cell therapy also carries risks such as infection and allergic reactions to medications. Additionally, ensuring the survival of stem cells in the avascular disc environment remains a challenge. Patients should carefully consider these risks and consult with medical professionals before undergoing stem cell therapy.
Patient Eligibility and Screening
Determining patient eligibility for stem cell therapy involves a thorough evaluation of existing medical conditions and the patient’s overall health. The screening process is critical in identifying whether a patient meets the specific health criteria necessary for receiving stem cell therapy.
Consulting medical professionals helps assess the potential risks and benefits of stem cell treatment for each patient. This ensures that only suitable candidates undergo the procedure, maximizing the chances of successful outcomes.
Summary
Stem cell therapy offers a promising avenue for treating chronic back pain and degenerative disc disease. By leveraging the natural repair processes of mesenchymal stem cells, patients can experience significant pain relief and improved tissue regeneration. Various sources of MSCs, such as bone marrow, adipose tissue, and umbilical cord tissue, provide versatile options for therapy.
With different administration methods, including intradiscal injections and intravenous infusions, patients can choose the most suitable treatment based on their needs and preferences. Supportive therapies further enhance the effectiveness of stem cell treatments, ensuring holistic recovery. As clinical trials continue to explore the potential of these therapies, the future of back pain treatment looks increasingly hopeful.
Frequently Asked Questions
What is the success rate of stem cell treatment for back pain?
The success rate of stem cell treatment for back pain varies, with recent studies indicating that approximately 40.7% of patients experienced positive outcomes after 6 months, while intradiscal MSC treatments showed a higher success rate of 69%. It’s essential to consider these mixed results when evaluating treatment options.
What are the negative side effects of stem cell therapy?
Stem cell therapy can lead to several negative side effects, including increased vulnerability to infections, low blood cell counts, bleeding, anemia, and complications such as graft-versus-host disease and veno-occlusive disease. It’s crucial to discuss these potential risks with your healthcare provider.
What are mesenchymal stem cells (MSCs) and how do they help with back pain?
Mesenchymal stem cells (MSCs) are specialized stem cells that can repair injured tissues. They aid in alleviating back pain by differentiating into cells that mend damaged intervertebral discs, reduce inflammation, and promote tissue regeneration.
What are the sources of mesenchymal stem cells used in treatments?
Mesenchymal stem cells (MSCs) are primarily sourced from bone marrow, adipose tissue, and umbilical cord tissue. Among these, umbilical cord-derived MSCs are noted for their higher proliferation rate and superior immunomodulatory properties.
How do intradiscal stem cell injections work?
Intradiscal stem cell injections work by extracting stem cells from the patient’s bone marrow and directly injecting them into damaged intervertebral discs, aiming to repair tissue, restore height, and alleviate pain. This approach promotes healing from within the disc itself.